Patients with pathological cardiac hypertrophy have a thickened heart that has a reduced ability to pump blood throughout the body. This debilitating condition is linked to inflammation, fibrosis and cell signaling disruptions, and leads directly to heart failure.
It is not uncommon and its molecular mechanisms – what
happens in our bodies that gives rise to this condition in the first place – is
not well understood. In science, when faced with persistent difficulty, new
approaches to studying a disease are in order.
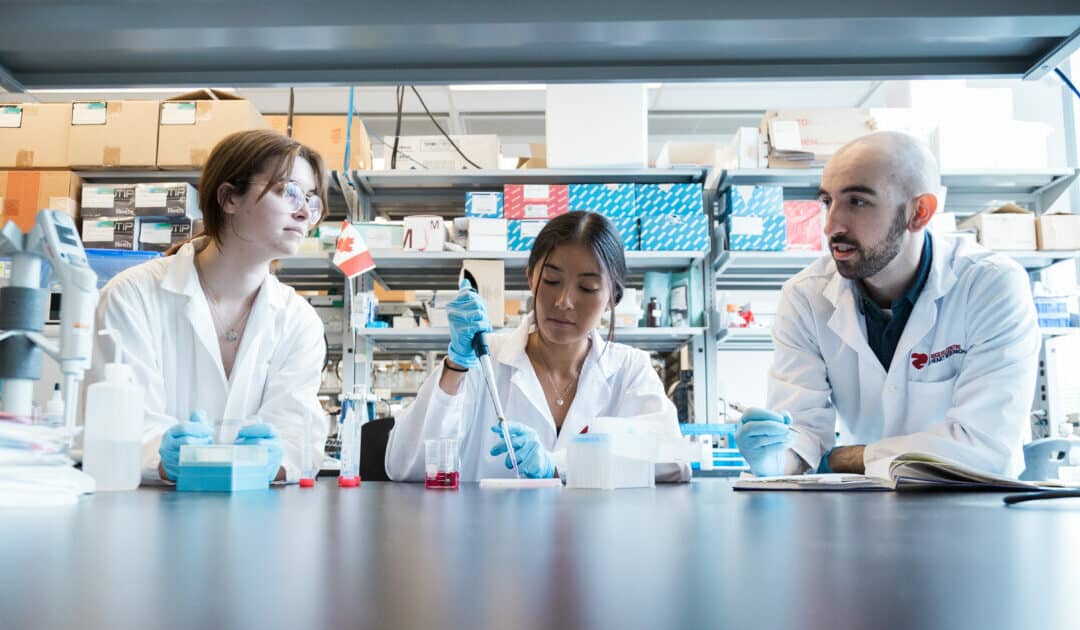
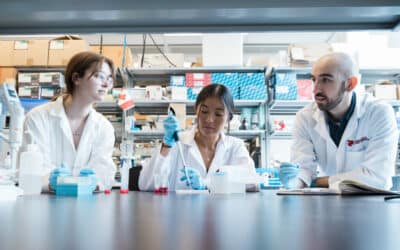
The world-class labs of Chris Yip, Anthony Gramolini, Craig
Simmons and Scott Heximer blended innovative imaging, physiology, biochemistry,
bioengineering and surgery in a new investigative approach to this disease.
(The latter three labs belong to the Ted Rogers Centre’s Translational Biology and Engineering
Program.)
The conventional approach in labs is to measure the level of
molecules and proteins, and how their fluctuations are tied to disease. This
time, in a bid to unearth new answers, these labs explored proteins in an
injured heart cell in a new way.
Tracking the movement
of proteins
“Our novel approach was to figure out where and if these
proteins moved around, reorganizing themselves,” says Sina Hadipour-Lakmehsari,
first author of the study
published in Nature Scientific
Reports. “It’s a different way of thinking about what happens inside a
cell, one where we can gain a greater depth of knowledge about the molecular
basis of this disease.”
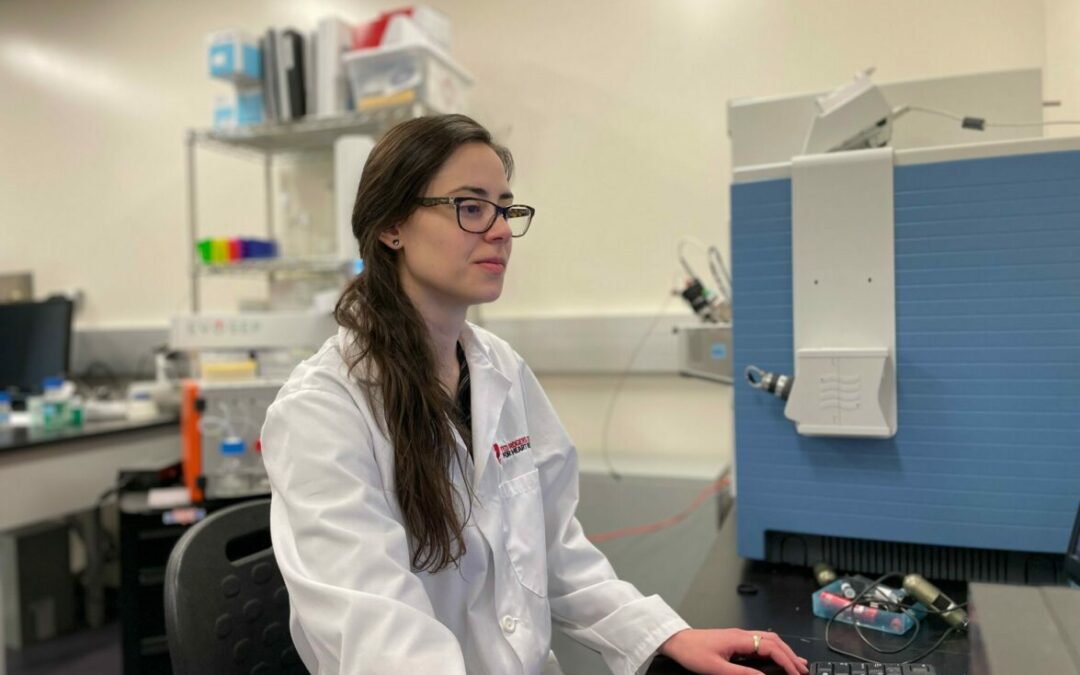
Imperative to the study was the use of dSTORM microscopy –
super resolution imaging that accurately detected those protein locations. That
element was led by Christopher Yip, Dean of the Faculty of Applied Science
& Engineering at U of T, who is a global leader in molecular imaging – a
field advancing at breakneck speed.
“By pinpointing the precise location of these molecules within
an affected cell, we can understand how the proteins are functioning,” says
Anthony Gramolini, Ted Rogers Centre principal investigator. “If there is any
change as to where those molecules are, it will have profound effects on that function
and suggest new clues to how this disease develops.”
What they discovered
about calcium
Cardiomyocytes (heart cells) require calcium to beat and contract. Some proteins are responsible for adding calcium if higher levels are needed, and some remove excess calcium from a cardiomyocyte. How calcium-regulating proteins are dispersed amidst pathological cardiac hypertrophy is the key finding of this study.
The team discovered that, after a heart suffers damage, cardiomyocytes start to widely disperse proteins that boost calcium levels in the cell. But those proteins that remove calcium appear to cluster together in tight groups, unable to effectively function. The result is a widespread calcium overload – which can play a role in the structural remodeling of cardiomyocytes and the progression of pathological hypertrophy.
“This is an important step to understanding what is
happening in cardiac hypertrophy, which hasn’t been yet considered,” says
Gramolini. “This multi-lab study is a direct result of the Ted Rogers Centre,
which enabled the collaborations of different experts, and has built momentum
in our scientific pursuit of heart failure.”
This model of investigation – tracking the movement of
proteins – is applicable to almost every disease. Getting the right researchers
working together can uncover new insights into human health simply by
reimagining the way we approach studies at the molecular level.
Image: 1. Upper panel – dSTORM super-resolution imaging of a molecular channel (RyR2) involved in calcium release in cardiomyocytes. 2. Bottom panel – dSTORM super-resolution imaging of a molecular protein (SERCA2A) involved in calcium uptake in cardiomyocytes.