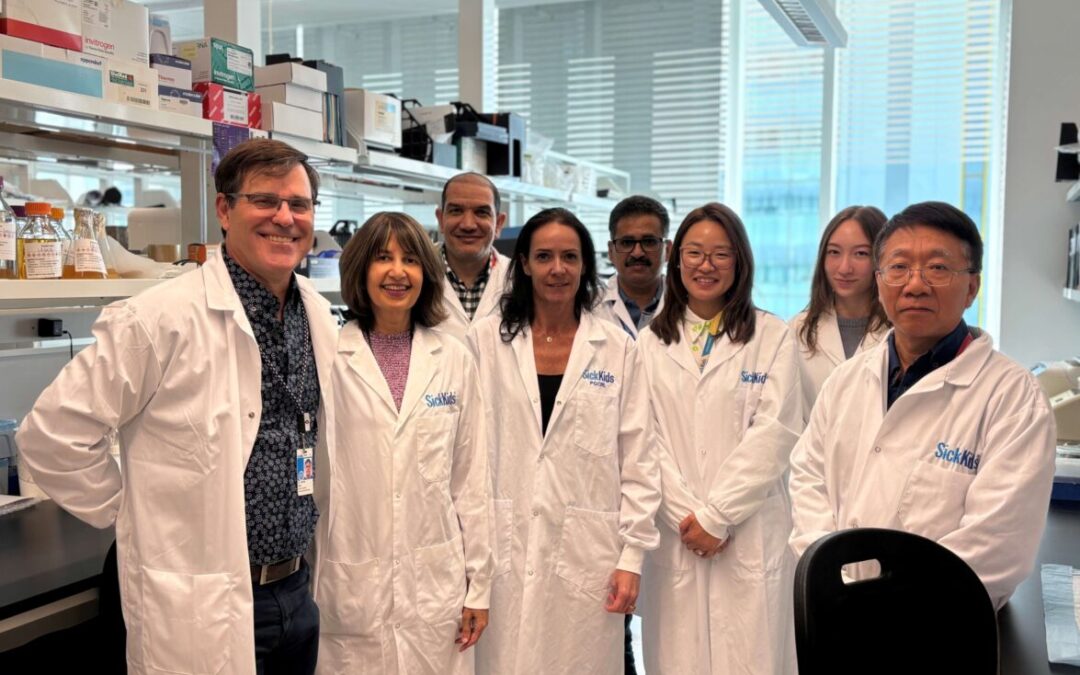
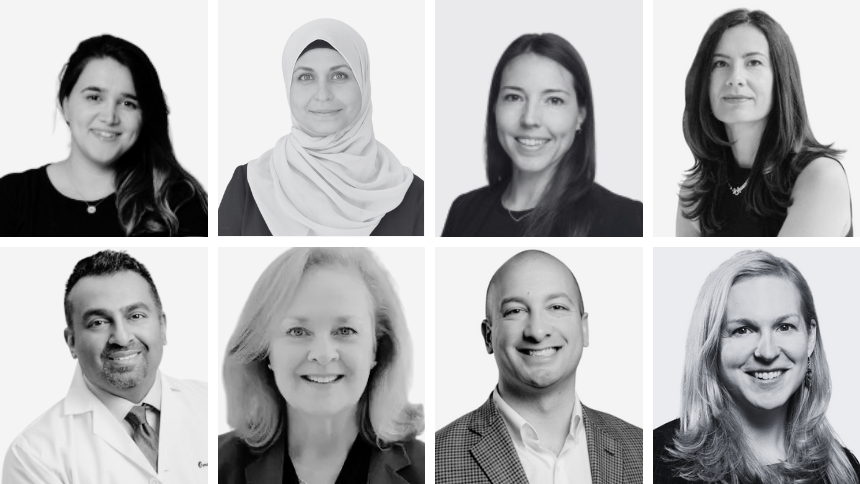
The ideal treatment team
Oncology and cardiology teams should work together – as they do in our cardiotoxicity prevention program – to help prevent any heart problems during cancer treatment.
“Cardio-oncologists” are cardiologists who assess cancer patients before treatment, monitor their symptoms and heart function during treatment, and provide long-term follow-up after treatment.
A key goal is to minimize interruptions to cancer therapy, as delays influence long-term outcomes. Where necessary, your cardio-oncologist can start medications to stabilize and improve heart function while the oncology team continues to administer cancer therapy.