With a mission to support novel approaches to managing and preventing heart failure, the Ted Rogers Centre for Heart Research uses its Innovation Fund to propel emerging research with great potential. In our 2024-25 Innovation Seed Grant competition, the Centre funded four such projects that span our three partners: The Hospital for Sick Children, University Health Network, and the University of Toronto.
Through these grants, research teams receive up to $100,000 a year – which is renewable for one year – if their projects show the greatest potential to transform cardiac care and have a clear path to actually serve patients in the clinic in not-distant future.
Introducing the winning projects in our 2024-2025 seed grant competition:
Bioengineered Decorin Eluting Microfibers to Treat Right Ventricular Fibrosis and Failure (DEFT-RVF)
Principle Name: Mark Friedberg | Collaborator: Paul Santerre
Objectives:
1. Create bioengineered microfiber mats (herein abbreviated to microfibers) coated with human recombinant decorin (hrDCN).
2. Deliver hrDCN-microfibers to the RV free-wall in survival rat PH and PAB models.
3. Define the impact of hrDCN-microfibers on RV fibrosis, stiffness and function in these animals.
Pulmonary hypertension (PH) is a serious condition caused by high blood pressure in the vessels of the lungs. This often leads to death because the right side of the heart, which normally pumps blood through the lungs at low pressure, struggles to handle the higher pressure. Over time, the right heart becomes damaged and scarred, making it weaker. To help solve this problem, Drs. Friedberg and Santerre are working with clinician scientists and engineers who have created tiny particle and fibre technology (patented nanostructures) to deliver targeted biomolecules (called decorin or DCN) to the heart. They discovered that these biomolecules, which help reduce scarring in the normal heart, are depleted in people with pulmonary hypertension. Dr. Friedberg says, “By replenishing these molecules to the heart muscle, we hope to allow the heart to pump better and improve survival in pulmonary hypertension.”
This project brings together expertise in cardiology, bioengineering, and imaging across SickKids, U of T, and UHN. Dr. Mark Friedberg, pediatric cardiologist and clinician-scientist at SickKids, is an international leader in RV physiology, remodeling, and fibrosis. Dr. Paul Santerre, Professor at the University of Toronto and Baxter Chair in Health Technology & Commercialization at UHN, brings expertise in biomaterial engineering, having developed injectable electro-spun fiber scaffolds that overcome the limitations of larger cardiac patches. This approach makes it possible to deliver high concentrations of DCN directly to the right ventricle wall in a tissue-friendly way. Dr. Simmons, TRCHR Scientific Lead at TBEP, contributes bioengineering expertise and advanced methods to measure right heart stiffness and tissue organization. Dr. Villemain, also at SickKids, adds expertise in ultrasound physics and, in collaboration with Friedberg, first used non-invasive ultrasound techniques to assess heart stiffness. Together, this collaboration integrates physiology, biomaterials, tissue biomechanics, and imaging to develop and test this biomolecule delivery technology as a potential therapy for right heart failure.
Targeting metabolism to treat heart failure: focus on mitochondrial trifunctional protein
Principle Name: Mansoor Husain | Collaborators: Anthony Gramolini and J. Rafael Montenegro-Burke
Objective: The objectives are to answer two key scientific questions: (i) does mitochondrial trifunctional protein (MTP) play a role in the development or progression of HF? (ii) is MTP a therapeutic target to prevent or treat HF?
Heart failure (HF) is a complex chronic disease, and current therapies have reached a plateau in slowing progression and improving outcomes. Recent advances in our understanding of “metabolic remodeling” point to new treatment opportunities. Clinical trials of drugs developed for type 2 diabetes and obesity, such as SGLT-2 inhibitors and GLP-1 analogs, have shown benefits for people with HF, likely because they also improve cardiac metabolism.
Building on this, researchers have identified mitochondrial trifunctional protein (MTP), a key enzyme in fatty acid metabolism, as a possible therapeutic target. Early findings suggest MTP behaves differently across HF subtypes: increased in HF with preserved ejection fraction (HFpEF), but reduced in post-heart attack models of HF with reduced ejection fraction (HFrEF). It remains unclear whether these changes are helpful or harmful, or whether they drive disease or are a consequence of it. Answering these questions could reveal whether targeting MTP offers a new way to treat HF, moving toward more precise, metabolism-based therapies. Principal Investigator, Dr. Mansoor Husain, expressed his outlook for the future, “This grant enables us to explore a promising new strategy to treat heart failure at its metabolic roots, offering hope for more effective and personalized therapies.”
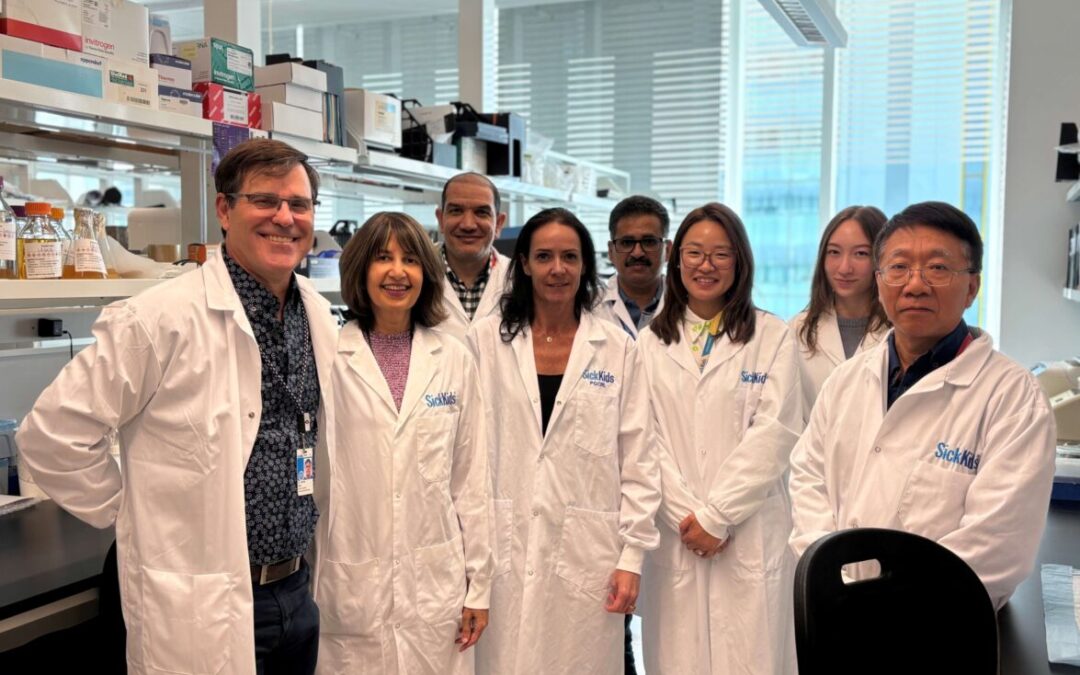
This project brings together expertise from two of the Centre’s partner institutions – University Health Network and the University of Toronto. At the UHN’s Toronto General Hospital Research Institute (TGHRI), Dr. Mansoor Husain’s lab specializes in disease modeling and translational cardiovascular research. At U of T’s Translational Biology and Engineering Program (TBEP), Dr. Anthony Gramolini brings expertise in mass spectrometry to study cardiac proteins and their modifications, and has already worked with the Husain Lab to identify protein signatures in mouse models of heart failure treated with GLP-1RA, SGLT2i, and a combination of both. Also at U of T, Dr. J. Rafael Montenegro-Burke, Canada Research Chair in Functional Metabolomics and Lipidomics at the Donnelly Centre, provides complementary skills in metabolomic and lipidomic analyses. Together, their combined approaches in pathophysiology, proteomics, and metabolomics make it possible to address the project’s questions about MTP and its role in heart failure.
RNA-based strategies to promote the engraftment of stem cell-derived cardiomyocytes
Principle Name: Michael Laflamme | Collaborator: Bowen Li
Objective:
1. Establish an optimized Circular RNA (circRNA) design for sustained protein translation in human pluripotent stem cell-derived cardiomyocytes (hPSC-CMs) in vitro and in vivo.
2. Define an optimal Lipid nanoparticle (LNP) formulation for circRNA delivery into hPSC-CMs.
When someone has a heart attack, part of the heart muscle dies and is replaced by scar tissue. Unlike muscle, scar tissue cannot contract, so the heart pumps less effectively. This often leads to heart failure, a serious condition that current treatments can only manage but not cure. One promising approach is to replace the damaged cells by transplanting heart muscle cells (cardiomyocytes) grown from stem cells (hPSC-CMs), which can form new, electrically integrated tissue and improve heart function in animal models. However, many of these cells die shortly after transplantation, limiting their effectiveness.
To address this challenge, Dr. Laflamme and his team are exploring a new kind of RNA called circular RNAs (circRNAs). Unlike regular linear RNA, circRNAs are more stable and can keep helpful proteins for longer. Preliminary findings show that circRNAs support stronger protein translation in transplanted heart cells, especially under stress conditions. This project will build on those results to test new circRNA designs and delivery methods using lipid nanoparticles, tiny fat-based particles similar to those used in COVID-19 vaccines, to bring circRNAs safely into transplanted heart cells. The ultimate goal is to boost the survival and function of these cells, making heart regeneration after a heart attack more successful.
“Our research team is very excited about the potential of combining cell therapy and cutting-edge RNA technologies as a novel strategy to treat failing hearts. We are grateful for this TRCHR Innovation Fund Seed grant, which will allow us to develop our approach and perform early proof-of-concept experiments,” says Dr. Michael Laflamme.
This project brings together expertise in stem cells, cardiac biology, and RNA therapeutics across UHN, U of T, and SickKids. Dr. Laflamme, Senior Scientist at UHN’s McEwen Stem Cell Institute and Canada Research Chair in Cardiovascular Regenerative Medicine, is a leader in generating human pluripotent stem cell-derived cardiomyocytes and testing them in preclinical models. Dr. Bowen Li, Assistant Professor at the University of Toronto and Canada Research Chair in RNA Vaccines, contributes specialized expertise in RNA design and non-viral delivery systems. Clinical guidance comes from Dr. Yau at UHN and Dr. Haller at SickKids, both cardiothoracic surgeons whose input will help with the translation and development of the therapeutic. The team’s complementary strengths position this collaboration to advance circRNA technology toward improving regenerative therapies for heart failure.
The safety and feasibility of neonatal ventricular septal defect repair
Principle Name: Mike Seed | Collaborators: Osami Honjo and Rafael Alonso-Gonzalez
Objective:
1. To determine the safety of neonatal primary VSD repair (<8 weeks after birth) by analyzing for serious AEs (SAEs) and adverse events (AEs) including perioperative brain injury assessed by MRI.
2. To determine the feasibility of neonatal primary VSD repair by evaluating patient recruitment and impact on health care services.
Ventricular septal defect (VSD) is the most common type of congenital heart disease. While once thought to have little impact on brain development, emerging evidence shows that children with VSDs are at increased risk of neurodevelopmental delays and disorders (NDDs). Studies have found lower cognitive and social functioning, more psychiatric conditions, and higher use of special education services compared to healthy peers. Brain imaging has revealed changes in brain structure linked to these outcomes, and registry data suggest that children with VSDs score lower on measures of cognitive, language, and motor development than children with other heart conditions previously associated with developmental risk.
Recent analyses indicate that the age at which surgery is performed may be an important factor. Later repair is linked with poorer early neurodevelopmental outcomes, raising the possibility that earlier surgery could be protective. However, early intervention is not without risks: a retrospective analysis at SickKids found no deaths among neonates who had VSD surgery compared to three deaths in the later-repair group, however the younger patients required longer hospital stays and more intensive support due to complications. These findings highlight the need to better understand the balance of risks and benefits of earlier VSD repair on both heart and brain outcomes.
Dr. Mike Seed asserts, “With most congenital cardiac patients now surviving infant heart surgery, we are increasingly focusing on their functional status, including neurodevelopmental outcomes. This study will examine the possibility that earlier surgery is protective against adverse neurodevelopmental outcomes resulting from heart failure during infancy, which is usually a period of rapid brain growth and development.”
This collaboration is anchored by SickKids, one of the world’s leading centers for pediatric cardiac care and extends across three other recruitment sites: McMaster Children’s Hospital, Children’s Hospital of Eastern Ontario, and London Children’s Hospital. Together, these institutions represent Ontario’s fetal and pediatric cardiology network. Dr. Mike Seed, pediatric cardiologist at SickKids, whose research explores how heart physiology in infants and fetuses influences brain development, leads the team. Complementing this expertise, SickKids’ surgical team, led by Dr. Honjo, brings extensive experience in neonatal cardiac surgery. The neurodevelopmental follow-up of patients will be overseen by neonatologist, Dr. Ly and neuropsychologist, Dr. Sananes, who provide critical expertise in evaluating developmental outcomes. Long-term outcomes, including mental health and parental stress, will be evaluated with input from Dr. Rafael Alonso-Gonzalez at UHN, who specializes in adult congenital heart disease. By combining pediatric cardiology, advanced imaging, surgery, neurodevelopmental evaluation, and long-term follow-up, this collaboration is uniquely positioned to clarify the impact of ventricular septal defect repair on child development.
2025-26 Innovation Fund
Our Innovation Fund is open to bench research, proof-of-concept development, and the clinical assessment of new innovations, allowing it to play a key role in propelling great ideas forward.
The Innovation Fund seed grants for 2025-26 will open at the end of 2025. To learn more, visit our Innovation Fund page.