Science has long assumed the heart could not regenerate itself. Yet in the past decade, we have discovered that the hearts of newborns babies actually can.
Now the big question: why don’t the hearts of adults have this same capability of regeneration? Our funded researcher, Sarah Dick is tracking down one promising lead under the supervision of Dr. Slava Epelman at University Health Network in Toronto.
Embryonic macrophages
Sarah is focused on specialized immune cells known as macrophages. She is building off seminal work in the field by Dr. Epelman, who helped differentiate the types of macrophages – including those we are born with, which he helped prove are key to cardiac recovery.
While many macrophages patrol the body looking for infections or injury, embryonic macrophages (EMs) play a vital role in the healing process. Since more than half of macrophages in the heart are embryonic in origin, they are directly tied to the heart overcoming an injury, like a heart attack. They are the ones in the womb and during infancy, helping literally build the heart.
After an injury
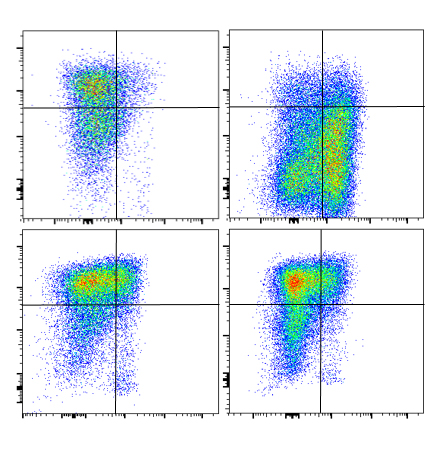
When the heart is injured, the body enters damage control. Macrophages from the bloodstream deliver inflammation to the site, which helps heal at first but that – if prolonged – can trigger serious complications like heart failure. Meanwhile, EMs in the heart are regenerative and believed to help the body create new cardiomyocytes (heart muscle cells) and new blood vessels to supply that muscle with oxygen.
The team in Dr. Epelman’s lab is interested in how these different macrophages interact, how cells are regulated and what communication occurs during the repair process.
Using novel tools, they have shown that by depleting EMs, the heart cannot repair itself well and instead worsens, leading to heart failure. The problem is that heart attacks wipe out a significant number of EMs – leaving any ability to regenerate weakened.
Sarah said that they want to find out what growth factors are linked to the proliferation of EMs which would promote an increase in their numbers. Can we administer such growth factors after a heart attack to help the heart repair itself? Are the macrophages from the blood, and the resulting inflammation, working against the proliferation of cells?
“Answers to these questions are vital not just for regenerating the heart, but also for cardiac remodelling,” Sarah said. “If it turns out we can’t regenerate the adult heart, we can remodel it in a way that allows it to function as well as possible. And save it from falling to heart failure.”
What’s next
Via an Education Fund grant from the Ted Rogers Centre, Sarah said she is able to leverage expertise of collaborators including Michael Laflamme and Milica Radisic, who are respective experts in cardiomyocytes and tissue engineering.
Research here could reveal how EMs interact and communicate with these types of heart cells. Could there be a growth factor, for instance, inside macrophages that sparks cardiomyocytes to proliferate and speed the healing process?
“I’ll be trying to figure out where we can intervene and help the heart’s innate ability to repair itself,” Sarah said.
(Image at top illustrates the transition from steady state, to inflammation after a heart attack, to a post-inflammatory state.)